The Humble Rubber Dam Leads the New Line-up of Infection Prevention & Control Defences in Dental Practice

A paradox: the famous Duomo in Florence had to wait 140 years for technology to become available to finish the ambitious soaring design of the cathedral’s dome. Yet, 150 years after the dental dam was invented, this life-saving device is still waiting for a nod of official approval. As baffling as it sounds, its use remains optional - even in the dental environment, where the risk of infection through the inherent presence of aerosols, fluids and contact is extremely high. Why have the regulators neglected to make the humble dental dam subject to the same rules as Hand Hygiene and Personal Protective Equipment (PPE) to close the loop of infection prevention and control?
Here is the thing. Despite the lack of clear rules on dental dam use, the responsibility, and consequences of failing to prevent infection spread, sits squarely with your dental practice. And dental dams are a lifeline between safer infection prevention and control practice and professional obligations. Why?
Because the very inventions that led to modern, faster, safer, and painless dentistry, the high-speed rotary instruments, such as handpieces or ultrasonic scalers and air-water syringes, have also led to producing high levels of dental aerosol and an even greater potential to transmit infection. This is currently one of the bigger challenges of dentistry.
There is no definitive, transformational solution to fully eliminate the problem of infection transmission in dentistry. COVID-19 has exacerbated the risks of airborne infections. Along with single patient use burs, dental dams stand on the frontline of protecting the doctor, the patient, and others.
Just one millilitre of blood can contain millions to trillions of major blood borne pathogens, such as Hepatitis B and C, and HIV. While data on COVID-19 is not currently available, as an airborne virus, it is smaller than blood and fluid particles. Therefore, in dental procedures, due to physical proximity to the patient, the risk of airborne transmission is considerably higher.
Dental dam or rubber dam is a thin, 150 mm square sheet, usually non-latex, or nitrile, used in dentistry to isolate the operative site (one or more teeth) from the rest of the mouth. Its many benefits, in addition to stopping saliva from interfering with the procedure, and preventing instruments and materials being inhaled, swallowed, or injuring the mouth, include preventing the spread of infections.
There are several dental treatments, where dental dams should be mandatory. Procedures include dental restorations, endodontic treatments including root canal therapy, fissure sealants, preparation of dental crowns, dental implants, and some veneer placements.
Yet, there is an astonishing lack of consensus amongst dental practitioners regarding the efficacy of rubber dam use. Hence, some use it routinely, but a large number of dentists do not utilise dental dams at all during procedures.
In March 1864 Dr Sanford Christie Barnum, a dentist from New York, who invented the rubber dam, wrote about his journey: “It was the result of my torment caused by saliva. I had passed hours, tired and distracted by my incessant struggle against unending saliva contamination. I had passed many sleepless nights obsessed over my sad failure….asking myself the same old question, that had yet to be answered: “How can I keep a cavity dry?” The answer revealed itself on the 15th of March 1864, while I was working on a lower left molar, in a mouth in which saliva was flowing everywhere. Desperate and eager to try a new idea, I made a hole in my protective napkin and placed it around the tooth. And that is how the rubber dam came to be.”
While the majority of critical breakthroughs in infection control in dental health and broader medicine coincided with the industrial revolution of the mid-19th century, 150 years later many of these scientific and practical inventions still have not been officially sanctioned.
1847 – Ignaz Semmelweis introduces washing hands for doctors between “performing autopsies to delivering babies” which results in instant reduction in the death rate.
1864 – Sanford Christie Barnum invented dental dam.
1865 – Louis Pasteur announces that microorganisms existed in the air.
1879 – Charles Chamberland and Louis Pasteur invent autoclave.
1884 – Robert Koch shows that TB could be transferred by aerosols, i.e. aerial droplets .
1889 – William Halsted introduces rubber gloves for theatre assistants / scrub nurses (note: not for doctors!).
1891 – W.D. Miller refers to toxic properties of saliva as a source of infection.
1899 – surgeons start wearing gloves, resulting in 100% drop in infections.
1931 – report shows that airborne infection of TB among dentists was higher than in other occupations.
1950s – invention of ultrasonic and high-speed turbine powered instruments and increased presence of aerosols brings more recommendations including use of rubber dam.
1987 – M.C. Martin shows that infection can be spread via dental unit water supply (DUWS) which led to the introduction of anti-retraction valves.

Diseases, infections and pandemics will always be part and parcel of humanity. What matters is the choices we make at any point of time to minimise the risks and to reduce the impact.
There are already several regulated ways to reduce or eliminate the risks of COVID-19 in dentistry, such as ceasing or postponing non-essential dentistry, and screening patients prior to dental treatment.
In terms of minimising the impact of aerosols, current recommendations include ventilation, strict cleaning, disinfecting and sterilisation procedures, and using pre-operative mouthwashes (containing chlorhexidine 0.2%, ideally under elevated temperature state). Other means focus on minimising the use of water spray syringes and using a carbide tungsten bur or, preferably, using single patient use burs of equivalent quality.

There is no such thing as post-COVID-19. The lesson to take away from this pandemic is that dental industry already has access to 150 years of thought leadership and most of the elements for effective infection control are available and constantly improved through technological innovation.
Making a real difference to infection prevention is about making the right choices of tools, supplies and equipment, as well as behaviours that support a safer future. Therefore, the industry and private practice in particular, must urgently rethink and adopt the new line-up of infection control measures. Here is the starting point.
In Australia, infection control obligations for dentistry are set out in Standard Precautions of the ADA Guidelines of Infection Control. Their goal is to guide dental professionals in adopting key focus points for infection control. This includes Hand Hygiene and PPE, consisting of Gloves, Masks, Eye protection, Gowns and Footwear.
The choices of PPE are subject to these Australian standards:
- AS/NZS 1337 – guides usage of reusable and disposable eyewear in dental practice.
- AS/NZS 4179 – guides procedures for use of sterile gloves.
- AS/NZS 4011 – guides usage of non-sterile gloves.
- AS/NZS 4381 – guides mask

After 150 years of proving its infection defence protection, the dental dam needs to lead the PPE defence line-up. The rationale for this has been abundantly Illustrated.
The dental dam was invented for one reason and this is to protect the dentist and the patient from infection. It was virtually the first element of PPE invented. Yet, ADA Guidelines for Infection Control only mention the dam as an ‘additional measure’ or in context of other products such as latex gloves. This may stem from the old attitude when doctors were more focused on protecting themselves rather than thinking of the patient’s exposure to infections.
As important as it is in infection prevention, the dental dam is a simple product, and prices can vary considerably. Key criteria for buying choices are economy, resistance to tearing and stretch or elongation capacity. While elongation capacity adds to the dentist’s and patient’s comfort, this comes with the trade-off risk of tearing, which causes time consuming complications and potential risk of infection.
Hence, it’s important to use reputable suppliers and brands for rubber dams. Reviews by independent, credible sources provide credibility to any marketing claims. One such product is Ongard ISODAM™, non-latex dental dam. When pitched against three other market leading brands, Crosstex, Hedy and Coltene, ISODAM™ won Dental Advisor’s top non-latex dental dam award for 2021.

Traditionally, the choices for PPE supply purchase have been based on the trade-offs between three criteria: degree of protection associated with product function, personal comfort or preference, and cost, the latter often being the deciding factor.
Using PPE products that are not genuine and therefore may not meet safety guidelines, poses a major risk to business and health. This consideration is especially valid when it comes to disposable masks and gowns. Just because they are disposable doesn’t mean they provide the necessary protection barrier for the dental team and the patient.
Amongst increasing concerns related to bloodborne and airborne pathogens, there is no room for complex decision-making. Protection of the surgical team and patients must become the priority focus. Any other choice than maximum quality of protection is false economy.
This is the kind of thinking the industry must change.
Here are some new considerations for choosing when making choices of key PPE elements listed under Standard Precautions in ADA Guidelines.
Masks:
Along with the ADA Guidelines, the use of masks in the dental industry is regulated by AS 4381: 2015 for single-use face masks. It now aligns with the North American ASTM F2100-11 and European (EN) 14683.
To clarify the confusion between P2 and N95 respirators, which are often used interchangeably, it must be remembered that Standard AS/NZS 1716: 2012 outlines the requirements for the P2 respirator, while N95 is governed by the USA NIOSH requirements.
COVID-19 has made wearing masks part of public life, dental teams must make a conscious decision which level of protection best applies to their activity and situation. Generally, there are three levels of masks that are suitable for dental settings.
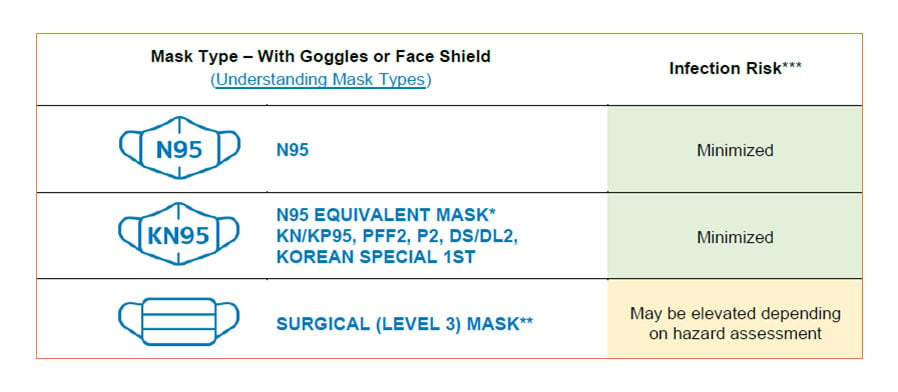 Not using effective masks in dental surgeries opens numerous serious risks:
Not using effective masks in dental surgeries opens numerous serious risks:
- Potential illness which may potentially be fatal
- Infecting others and causing infection outbreak
- Emotional stress
- Loss of income and / or employment
- Closure of dental facility and associated cost
- Lost trust by patients and loss of revenue
Gowns:
It’s important to realise that costs are generally comparable for functional equivalencies, when sourced from genuine, reputable suppliers. If the price is too good to believe, it should ring alarm bells.
In the absence of a dedicated Australian standard for dental gowns, ANSI/AAMI PB70 standard provides the best guide to evaluate the barrier effectiveness of surgical gowns.
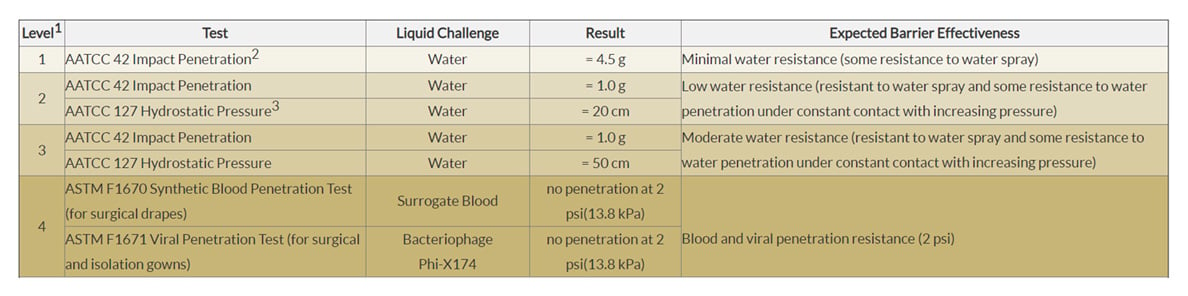
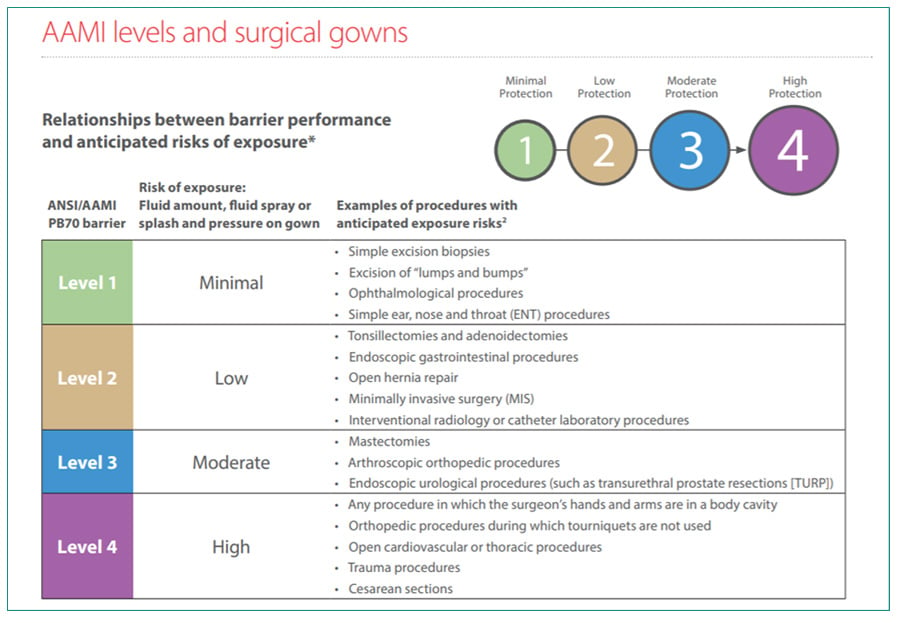
Based on standardized tests, ANSI/AAMI PB70:2012 outlines four levels of barrier performance with level 1 offering minimal protection. Levels 1 to 3 provide a scale of protection against liquid penetration. Level 4 extends protection to airborne pathogens.
Established, reputable suppliers provide a range of gowns across all levels of protection requirements from different, accredited manufacturers. Ark Health, for instance, offers surgical gowns from super cost-effective Everyday Essentials, to specialist Sentry Medical sterile and non-sterile gowns that cover every level of protection.
Gloves
The choices of surgical and non-surgical gloves for dental practices are abundant and the same principle applies. Buying from reputable sources that meet industry standards ensures your legal compliance. Poor quality gloves pose a serious health threat to the dental professional performing any dental procedures.
As the latex sensitivity is a recognised a serious health concern and addressed in ADA Guidelines, it should be included in buying criteria.
Many good suppliers, such as Ark Health, provide a selection of non-sterile latex and non-latex nitrile gloves.
Conclusion
If you can take one idea from this article, it is to be aware of the false economy when choosing any Personal Protection Equipment. Potential risks to health, business and reputation well outweigh any monetary gains. In this context we recommend that in choosing your supplies, consult reputable distributors and don’t just compare the price but also demand proof of performance of their PPE products.
If you need extra information or assistance in making PPE choices for your practice, call 1800 422 227 to speak to an expert. And feel free to visit https://www.arkhealth.com.au/.