SYNTHETIC BONE GRAFTS: COMMON MYTHS 3
Please enjoy the final installment of the Synthetic Bone Grafts: Common Myths 3 series by Dr Peter Fairbairn from EthOss.
This article examines how synthetic bone graft material has changed over the years and asks whether using it still requires a high level of technique sensitivity.
Please let us know what you thought of this Common Myths series here. We'd love to hear your feedback!
“Synthetic bone grafts are too technique sensitive, they don’t work for the ‘normal’ implantologist”
This is an interesting area, as this myth is largely grounded in truth. I won’t deny that previous generations of synthetics could be a bit technique sensitive – I’ve been using them personally for 20 years and have experienced the evolution first-hand.
Synthetic bone graft materials have come a long way in recent years. Our understanding of the porosity, surface area, particle stacking and particle shape has increased dramatically, and these have all been factored into the design of modern B-TCP products such as EthOss.
Why is this important?
It has helped the materials become much more predictable, easy to handle and overcome many of the issues with “technique sensitivity” that were associated with previous generations of synthetics.
Modern B-TCP is not the same material that many people may have trialled before, and if you have had poor experiences with old-fashioned synthetics then I would encourage you to have a look at these new materials. The difference is massive.
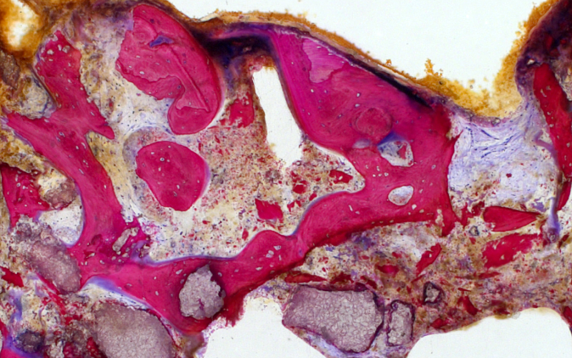
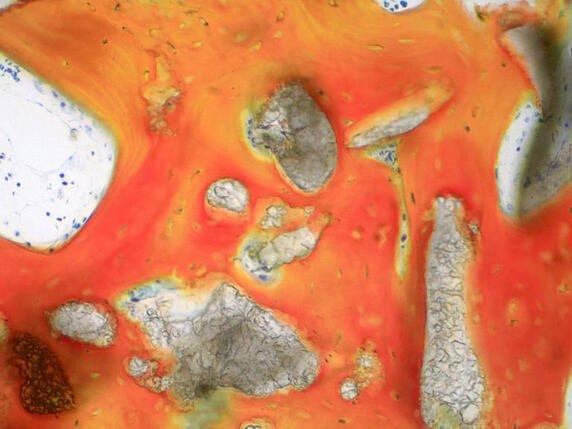
Above first: Human bone biopsy after twelve weeks of healing. Socket grafting with β-TCP/CS (EthOss). Newly-formed bone trabeculae (NB) and disintegrating EthOss particles (EO). Histomorphometric analysis of the sample revealed 48.12 per cent newly formed bone and 8.11 per cent residual EthOss particles.
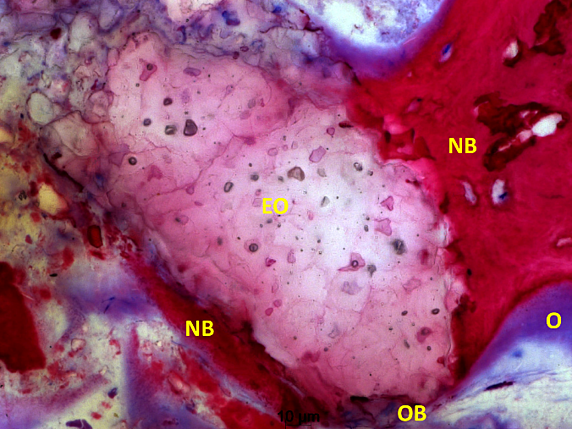
Above centre: Histological picture showing the breakdown and the reaction of a β-TCP/CS (EthOss) granule (EO) in newly-formed bone formation after ten weeks of healing. The β-TCP/CS particle is partially disintegrated, allowing osteoblasts (OB) to actively form osteoid (O) and add new bone trabeculae (NB) in contact and inside the pores of the bioactive grafting material.
Above last: Human bone biopsy after ten weeks of healing. Socket grafting with β-TCP/CS (EthOss). Histological picture showing tight integration of β-TCP/CS particles (Gr) in newly-formed bone trabeculae (NB). Van Gieson’s staining.
So are new, modern synthetics still “technique sensitive”? It depends on your perspective. They are not xenografts and cannot be treated as such, they do require some slight refinement in protocols and techniques if you are used to traditional materials. But I generally find the new techniques are simpler and easier, allowing me to achieve very high consistency and reliable results in my practice (the Protocol I published in 2015 contained over 600 grafts with a 99% success rate).
The biggest difference is obviously the membrane. With a material like EthOss, which contains an integrated “pseudomembrane”, you don’t need to use a separate collagen membrane. Using a separate collagen membrane may inhibit the blood flow to the site and therefore the body’s ability to heal – by removing this barrier we are making it easier for the body to heal itself.
It is also not necessary to over-pack the material as you shouldn’t see any loss in volume – this should contribute towards making primary closure easier (however if there is still an exposure then I would recommend you look at your flap design and move the opening either slightly to the palatal or buccal aspect, ensuring the opening isn’t over the graft).
It is also important to clean the site properly – any degranulation tissue can be an issue. This is not a unique problem to synthetics though and should be regarded as good surgical practice with any material.
By making these small adjustments anybody can achieve fantastic results with modern synthetics – it’s why they are the “fastest-growing” type of graft material (source: https://www.marketsandmarkets.com/Market-Reports/dental-bone-graft-substitutes-market-159678690.html). The benefits of the materials – full resorption in line with new host bone formation, biocompatibility, integrated membrane, no patient / ethical issues – are significant compared to traditional xenografts and allografts. They are also very flexible and can be used with a wide variety of techniques – have a look at our Case Studies Library for a range of examples:
1) Sinus augmentation lateral window – Dr Peter Fairbairn
2) Immediate dental implant placement – Dr Oliver Lys, Switzerland
3) Two wall periodontal bone graft – Dr Renukanth Raman, Malaysia
4) Sinus lift and periodontal grafting – Dr Peter Fairbairn
Writing these blogs surrounding “common myths” has been enjoyable – these questions tend to pop-up wherever I lecture or visit anywhere in the world and it’s refreshing to see more and more people moving down the synthetic route.
If you still have questions about the techniques surrounding EthOss then visit our EthOss Case Studies group on Facebook. Here you can see a wide range of different techniques from clinicians all over the world showing how they achieve great results using the material.